Diabetic retinopathy is one of the more common complications seen in people who have type 1 and type 2 diabetes. Recent studies have found that fifty percent of people with raised sugar levels, in the pre-diabetes stage, are at risk.
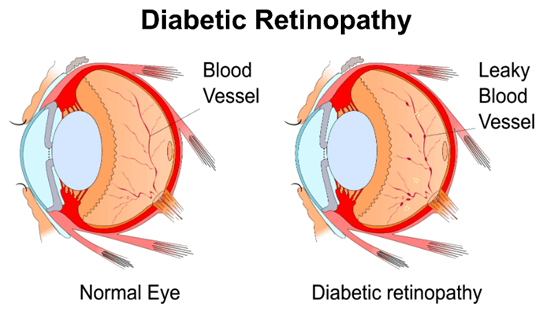
Diabetic retinopathy is simply a condition that occurs when elevated sugar levels damage the blood vessels in the retina. The retina is the upper layer tissue located behind the inner portion of the eye. The retina is the light-sensitive part of the eye and is crucial for healthy eyesight. This is why blindness often occurs when the retina is damaged. Sadly, there is very little warning or symptoms before the onset of diabetic retinopathy. This makes it critical for all diabetics to have an eye exam at least once in a year.
Diabetic retinopathy has four stages, and if detected early enough there are treatments to halt the progression of the disease so that it does not lead to blindness. If you should see spots of blood, or spots floating just in your vision, even if it only happens once, go to eye doctor pembroke pines and have a complete eye exam. Do not wait, or further damage to the eye may occur. Sometimes these spots will clear up without any treatment, but hemorrhaging can occur at night, and blurred vision is the likely result.
Here are the four stages
1. Mild Nonproliferative Retinopathy – The retina has many small blood vessels, and small microaneurysms or swelling occur.
2. Moderate Nonproliferative Retinopathy – The swelling gets worse until it completely blocks the blood vessels go into the retina.
3. Severe Nonproliferative Retinopathy – The blocked vessels become more swollen, which deprives several parts of the retina of their vital blood supply. To compensate, the retina asks the brain to grow more blood vessels.
4. Proliferative Retinopathy – In the fourth and final stage, new blood vessels develop, but they are fragile and too frail to cope with blood flow. Once these blood vessels leak, the end prognosis is the loss of vision or blindness.
Another complication that arises from diabetic retinopathy is macular edema. The macular is the center of the retina and it controls straight ahead and sharp vision. Statistically, fifty percent of individuals with proliferative retinopathy are said to also have macular edema.
Diabetic Retinopathy is considered the worst eye disease that most people could ever get. This is because in the first stages of this disease, one may not notice any changes in his or her vision, but it will eventually get worse and even cause blindness. That is why the disease is a major cause of blindness among many adults, as well as the most common eye disease in diabetics.
Diabetes is characterized by high blood sugar levels. The hormone insulin is responsible for converting the sugar level, or glucose in blood, into energy for the body to use as it sees fit. Excessive blood sugar can have serious consequences to one’s health. Thus, diabetes is a disease that interferes with the body’s ability to process sugar by impeding or destroying the ability of insulin to work in the body. A person with diabetes can suffer from many ancillary diseases that are a consequence of diabetes.
Diabetes is a dangerous disease. It can cause kidney failure, stroke, and heart disease. But most people are not aware that it can cause blindness or sever vision loss. The eye’s blood vessels will become weak if the blood sugar in our body is not controlled well. There will be fluid leaks in the eyes which eventually will cause the blood vessels to close, thus stopping the flow of blood to the retina. New but fragile blood vessels will form, but because they are so fragile, blood will leak into the eyes and cause severe vision problems and blindness.
Symptoms that will affect your eyesight
It’s not always easy to recognize the symptoms of this disease in the early stages, but there are some warning signs that you should look out for. These include:
- Dots of blood floating in your line of eyesight.
- Bleeding in your eyes from a hemorrhage. This often occurs after sleeping.
- Periodic or permanent swelling of the retina.
- Vision impairment, which can include blurred vision after some of the other symptoms have disappeared.
- Total vision loss.
In the early stages of this eye disease, there are no symptoms, which is why you need to have a thorough eye examination every twelve months.
As eye damage progresses you may notice:
- Poor night vision
- Vision loss
- Blurred vision
- Spots or floaters in your vision
- Shadows or missing vision areas.
Everybody that has diabetic issues is in danger of developing diabetic retinopathy, although not all diabetics may develop it. During the early stages, the patient might not discover any kind of changes in their eyesight, but you have to be aware that it can lead to vision loss and even permanent blindness.
One effective form of treatment for this particular eye problem is a vitrectomy. This is a surgical treatment that removes the vitreous humor gel from the eyeball. During this process, the gel within the eye cavity is removed. This allows the surgeon to access the retina to do things such as remove scar tissue, fix retinal detachments or treat macular holes. These procedures can help improve eyesight.
Another treatment for diabetic retinopathy is laser treatment. During the laser surgical treatment, blood vessels are made thinner to avoid the leakage of blood that may trigger vision loss. This is procedure is suitable for individuals with blood vessels that are not yet in the bleeding stage.
Diabetic retinopathy might be exacerbated and trigger blindness if treatment is not sought quickly. In some instances, if the patient possesses a late stage of retinopathy, and laser treatment or vitrectomy is not done, it can lead to continuously deteriorating eyesight.
To keep your eyes in the best shape possible, and catch any signs of eye disease early, make sure you see an optometrist or ophthalmologist at least once a year or whatever frequency your doctor may advise.
While it is unusual for most adults to suffer from glaucoma, those with diabetes are at a higher risk of developing it – in fact, twice as likely. Glaucoma is a result of damage to the optic nerve due to an increase in fluid pressure in the eye. This will eventually lead to loss of vision and blindness.