What is a liver transplantation?
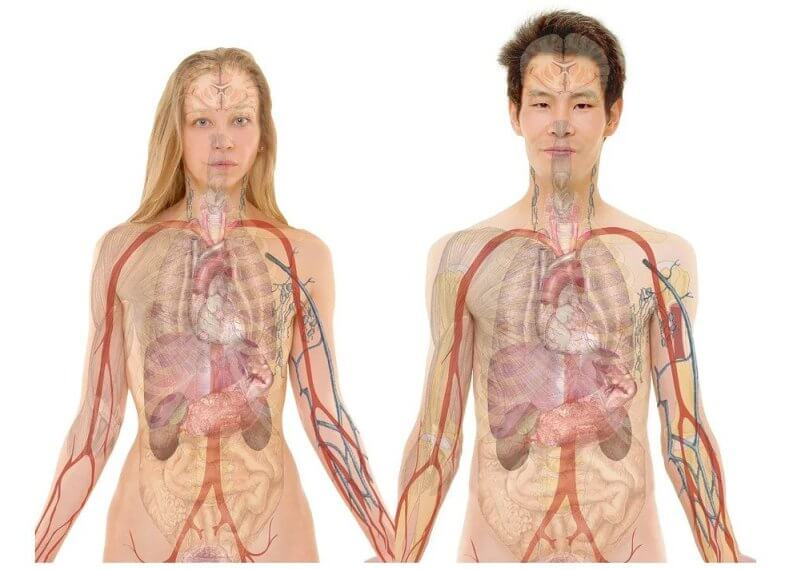
The liver is an important organ, whose main function is to filter the blood that circulates in the body and to produce bile, which helps with the digestion of food in the small intestine.
Liver transplantation is a surgical procedure performed with the objective of removing the liver that no longer performs its functions in the body and replacing it with a healthy liver from a deceased donor or a part of a liver from a living donor.
This procedure is necessary when a patient has chronic liver failure due to a disease or health complication. The liver performs some of the most important functions in the body, such as:
- Processing of nutrients and hormones.
- Production of bile for the absorption of fat, cholesterol and fat-soluble vitamins.
- Production of proteins for blood clotting.
- Elimination of bacteria and toxins in the blood.
- Prevention of infections in the body.
- Regulation of immune responses in the body.
- Storage of sugars, fats, iron, copper and vitamins.
What are the main causes of liver damage?
The main causes of liver damage are:
- Alcoholic hepatitis.
- Viral hepatitis.
- Cirrhosis.
- Liver cancer.
What are the different types of liver transplantation?
Since donor livers are difficult to find, and there is a long waiting list for patients, a rigorous evaluation is performed to determine who is suitable for a liver transplant. A stem cell transplant from another person (a donor) is called a donor stem cell transplant. The medical term for this is an allogeneic stem cell transplantation or a bone marrow transplant.
A patient is considered an ideal recipient if their lifespan would be shorter in the absence of a transplant and if there is at least a 50% chance that the patient will survive for five years after transplantation. The different ways a liver transplant can be performed are:
- Orthotopic whole liver transplantation. It is the most common type of transplant. It consists of the removal of the diseased liver of the patient and the implantation of the entire liver of a deceased donor in the same anatomical place.
- Orthotopic partial liver transplantation. Partial liver transplantation involves the removal of the diseased liver and the placement of a piece of the donor liver (right lobe or left lobe) in its place. This is done when the transplant is performed using the split technique or it is a living donor transplant. After approximately two months, the transplanted liver fragment regenerates and regains its full size and full functions.
What diseases may need a Liver Transplant?
Despite the fact that liver transplantation is, theoretically, the treatment of liver diseases in all patients with severe and irreversible liver and bile duct diseases, it is the hepatologist from liver company who determines the indication for a transplant.
In general, the diseases that most commonly require transplantation are: chronic cholestatic diseases (primary biliary cirrhosis; primary sclerosing cholangitis, niliary atresia (typical children disease); cirrhosis of non-biliary origin due to hepatitis B and C virus, alcoholic, autoimmune, non-alcoholic steatohepatitis (NASH), cryptogenic; liver tumors (hepatocellular carcinoma); acute liver failure (acute viral hepatitis, acute toxic-drug hepatitis, acute liver failure of undetermined cause); metabolic diseases (hemochromatosis; Wilson’s disease; tyrosinemia, glycogenesis) and other diseases (Budd-Chiari syndrome; Caroli disease).
Post-intervention recovery
After liver transplant surgery, the recipient patient should notice an almost instantaneous improvement compared to the symptoms previously caused by the diseased liver. Patients can often return to normal activities in a matter of months, but full recovery can take much longer. A transplant patient will need to take immunosuppressive medications for the rest of his life to prevent the body from rejecting the donor liver.
Risks related to liver transplantation
There may be risks after liver transplant surgery, although the prognosis is good in most cases. About eight out of ten liver transplant patients live at least another five years, and many even live for more than 20 years.
The main problems related to liver transplant surgery are:
- The donated liver is rejected by the body.
- The donated liver does not work at first, resulting in a new transplant that will be performed immediately.
Hemorrhage. - An increased risk of infection.
- Blood flow problems to and from the liver.
- An increased risk of skin cancer.
FAQ:
Who can be a living liver donor?
Any person, over 18 years of age and under 55 years of age, in full use of mental faculties who, after being adequately informed of the benefits and risks of the donation process, has the firm will to be considered a liver donor and who, from a medical point of view, he is totally healthy, in accordance with very strict criteria established in living donation protocols.
The donor and recipient must be compatible in terms of blood type.
Most donors are relatives (parents, siblings, spouses, other relatives), although they can also be people with emotional ties to the recipient (friends, co-workers). The decision to donate must be free from coercion and pressure from the environment. The donated organ is a free gift. The law does not allow the sale of an organ for transplantation.
Are elderly people dismissed as cadaveric donors?
The age of the donor, in itself, is not a contraindication for transplantation. Apart from age, in a potential organ donor, the general condition of the donor, how their organs function and the appearance of each organ during the extraction should also be evaluated.
How is the compatibility between donor and recipient determined?
The compatibility between donor and recipient is determined according to blood group and body weight.
Blood type. There must be ABO blood group identity between the transplant patient and the liver donor. Thus, for example, group A patients can only receive organs from donors of the same group A. In living donor transplants, the blood group can be identical or only compatible. In this case, for example, a group A patient may receive a liver transplant from a donor of blood group A or O.
Body weight. In order for the volume of the transplanted liver to be neither too large (there could be problems fitting in the transplant recipient’s abdomen) nor too small (it could be insufficient for the life of the patient), there needs to be a certain similarity of body weight between the patient and his donor. This factor is especially important when the donor is a living donor from which only one lobe of the liver can be obtained.
Can I get pregnant after a liver transplant?
Women of childbearing age may not menstruate for a time after transplantation, although it does not mean that they cannot become pregnant, as they continue to ovulate. During the first year after transplantation, it is very important that the patient does not become pregnant. Starting from the first year, the possibility of pregnancy should be evaluated individually by your hepatologist and gynecologist.